Heel Pain Causes & Treatment Options
The 12 most common causes of heel pain in adults and how they are diagnosed and treated.
Preferred Foot & Ankle Podiatry Clinic in Arizona
The Two Most Likely Causes of Heel Pain in Adults are Plantar Fasciitis and Achilles Tendinitis.
But these aren’t the only causes of adult heel pain. Since these are the most common causes (Plantar Fasciitis and Achilles Tendinitis), we want to focus on them first, but the full list of 12 can be found below (or you can jump to that section here: 12 common causes of heel pain).
This article has been written in collaboration with foot and heel pain doctors, Dr. Mikkel Jarman and Dr. Brent Weintrub. The information has been derived from both clinical studies and inhouse patient statistics, the content is credible and verified, but still should only serve as information only and not an official diagnosis. For an official diagnosis we always recomend seeing a podiatrist or foot specialists that truly understands the intricacies of the bones, ligaments, muscles, and other tissues of the foot and ankle to accurately diagnose the cause of your heel pain.
Having said that, if you are suffering from heel pain, or just want to learn more about it, we still highly recommend this page as an up-to-date and accurate source of information. Let’s jump in (pun intended)!
Important Consideration Regarding Children’s Heel Pain*
It’s important to note that heel pain in children is not the same as adult heel pain. Heel pain in children is generally (but not always) the result of conditions related only to children like Sever’s disease. Learn more about children’s heel pain here: Heel Pain in Children.
Plantar Fasciitis
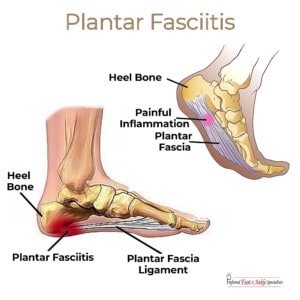
Plantar fasciitis is marked by a sharp, stabbing pain along the bottom of the foot. It’s caused by inflammation of the plantar fascia, which is the thick band of tissue connecting your heel bone to your toes.
Typically, plantar fasciitis hurts most when you first put weight on your foot after a long period of rest, such as first thing in the morning or after sitting at your desk for a while. Pain typically decreases after you walk around for a bit, but may return, particularly after long periods of time spent standing.
The risk of developing plantar fasciitis is highest among runners, people whose footwear does not provide adequate support, and those who are obese.
Achilles Tendinitis

The Achilles tendon connects your calf muscles to your heel bone. Achilles tendinitis occurs when this tendon is strained or injured due to overuse. Pain is typically mild at first, increasing in intensity over time.
The condition commonly strikes runners when they increase the length and/or intensity of their workout. As you get older, your risk of Achilles tendinitis is higher if you aren’t regularly active, such as those who play a sport only on the weekend.
Although self-care guided by your podiatrist is typically prescribed to treat tendinitis, if your Achilles tendon ruptures or tears, you may require surgery to return full function to the foot.
Plantar fasciitis videos
Conservative Plantar Fasciitis Treatment for Acute Conditions
Both Dr. Jarman and Dr. Weintrub prefer to explore conservative treatment options first, reserving surgery as a last result. Dr. Weintrub shares conservative treatment options in this video.
Determining Whether Plantar Fasciitis is Acute or Chronic
Dr. Weintrub with Preferred Foot & Ankle Specialists discusses Acute Plantar Fasciitis versus Chronic Plantar Fasciitis, and the different treatment options for both.
Heel Pain is Never Normal
Heel or foot pain is never “normal” and should not be ignored. It could be something as simple as an overuse injury but it may also be the symptom of a condition requiring medical treatment, such as a stress fracture or ruptured tendon. It’s important to consult with a heel pain podiatrist who has experience treating heel pain.
The 12 Most Common Causes of Heel Pain in Adults
- Plantar Fasciitis is caused by the inflamation of the plantar fascia, a thick band at the bottom or the foot that connects the heel bone to the toes.
- Achilles Tendinitis occurs when the Achilles tendon (connects calf muscle to heel bone) becomes strained or injured due to overuse.
- Stress fractures occur most often in the weight-bearing bones of the foot and lower leg, such as the calcaneus (heel bone) and tibia (shin bone). Calcaneal stress fractures are most commonly caused by overuse, such as activities that require a lot of running or jumping, and in conjunction with other injuries, like a sprained ankle.
- Calcaneal cysts form on the heel bone and may be painful or painless. Typically, the cyst only becomes painful when it presses on surrounding tissues. Painless calcaneal cysts are fairly commonly and are usually discovered during a routine foot examination.
- Baxter’s nerve entrapment occurs when the small branch of the plantar nerve (the eponymous Baxter’s nerve) becomes pinched between two muscles. Also known as Baxter’s neuritis, the condition may also be caused by chronic plantar fasciitis or a calcaneal bone spur.
- Short flexor tendon tears occur when the tendons along the bottom of the foot (the ones that help you bend your toes) rupture or tear. They’re usually caused by ankle sprains and strains.
- Plantar fascia ruptures are caused by either chronic pressure or intense, acute pressure on the plantar fascia – the ligament that supports the arch of your foot. When these fibers tear, it typically results in an intense, burning pain. (See Jeff’s testimonial in video section below).
- Gout is a form of arthritis that most often effects the big toe, not the heel – although your entire foot will likely hurt. Sudden attacks of gout occur when urate crystals (uric acid) build up in the joint, causing inflammation and intense pain. The joint typically swells, becoming red and tender, and often feels hot. A gout attack may leave your toe joint feeling so tender that any amount of pressure, even a sock, feels intolerable.
- Systemic arthritis attacks the joints of the body, including your feet. The three most common types of arthritis are osteoarthritis (a wearing down of the cartilage protecting your joints), rheumatoid arthritis (an autoimmune disorder that causes your immune system to attack your own body), and psoriatic arthritis (a condition typically limited to people who have psoriasis).
- Soft tissue masses may form in the foot and ankle. They’re rarely dangerous but they can be painful. The most common soft tissue mass in the foot and ankle area is the ganglion cyst.
- Tarsal tunnel syndrome is the result of tibial nerve compression (the tibial nerve runs down the back of your shin and into your foot). When you feel pain, numbness, or tingling on the sole of the foot, it is usually because of tibial nerve compression. Tarsal tunnel syndrome is most often caused by an ankle injury.
- Infracalcaneal bursitis occurs when the fluid-filled sac (known as the bursa) below your heel bone becomes inflamed. The bursa helps reduce friction between connecting tissues. Prolonged or excessive movement may cause this painful inflammation.
The Number 1 Cause of Adult Heel Pain: Plantar Fasciitis
Plantar fasciitis is the most common source of heel pain in adults. It is caused by inflammation of the plantar fascia, the ligament that runs along the bottom of your foot and connects the toes to the heel.
The plantar fascia supports the arch of your foot and helps absorb the shock of impact when you walk or run. When you place too much tension on this tissue, it stretches and may become inflamed or even tear or rupture.
Symptoms of plantar fasciitis
The most common symptom of plantar fasciitis is a sharp pain that starts near the heel and runs along the bottom of your foot. Typically, pain is worse during your first steps in the morning or after long periods spent sitting. It then dissipates once you’ve walked around for a bit. Pain may also be triggered by standing for long periods of time.
Plantar fasciitis risk factors
Although there is still no obvious cause for plantar fasciitis, we do know certain risk factors increase your chances of developing the condition.
- You’re more likely to get plantar fasciitis between the ages of 40 and 60.
- Activities that place a lot of stress on the foot – particularly the heel – raise your risk. Running, aerobics, and dancing are common culprits.
- Having high arches or flat feet also increase your risk of plantar fasciitis, particularly if they lead to an abnormal gait (walking pattern).
- Obesity adds extra stress throughout your body but particularly your feet.
- People whose jobs require them to spend a lot of time on their feet – teachers, factory workers, retailers, etc. – are more likely to develop plantar fasciitis.
Diagnosing plantar fasciitis
Diagnosing plantar fasciitis involves taking your medical history and conducting a physical examination to check different areas of the foot for tenderness. Imaging tests like MRIs and x-rays may be performed, but this is mainly to rule out other causes for your foot pain, such as a stress fracture.
Plantar fasciitis treatment
Most plantar fasciitis patients do well with conservative treatment (i.e., non-surgical). This may include:
- Over-the-counter pain relievers like ibuprofen
- Resting, icing, and stretching the affected foot
- Changes to foot gear for better support
- Custom orthotics to help distribute weight more evenly
- Physical therapy to help stretch the plantar fascia and strengthen the muscles of your lower leg
- Night splints that help stretch the calf and arch of the foot
What Causes Achilles Tendinitis?
Either repetitive or acute strain on the Achilles tendon may cause inflammation known as Achilles tendinitis. You rely on your Achilles tendon to walk, run, or even stand on your tiptoes, so it gets a lot of use.
Symptoms of Achilles tendinitis
The pain of Achilles tendinitis usually starts as a mild ache just above the heel or at the back of the leg. Pain may be more severe after more prolonged or intense activity. You may also feel more tender or stiff after long periods of inactivity, with symptoms easing after you walk around for a bit.
Call your doctor immediately if pain is severe or persistent, as this is may indicate a torn or ruptured Achilles tendon.
Achilles tendinitis risk factors
Risk factors for Achilles tendinitis include:
- Gender: Men are more likely to develop Achilles tendinitis.
- Age: The Achilles tendon weakens with age, making injury more likely.
- Flat feet: Low arches place more strain on the Achilles tendon.
- Obesity: Again, being overweight puts additional strain on your body in numerous ways, particularly the weight-bearing structures of your feet and lower legs.
- Inadequate shoe support: If you’re a runner, you need to replace your footwear regularly – at least every 300-400 miles.
- Exercising in cold weather: Risk of Achilles tendon injury is higher in cold weather than when it’s warm.
- Hilly terrain: Running or walking on uneven or hilly terrain also increases the risk of injury.
- Certain medical conditions: Both high blood pressure and psoriasis increase your odds of developing Achilles tendinitis.
- Fluoroquinolones: An antibiotic prescribed to treat certain types of bacterial infections, fluoroquinolones increase your risk for tendinitis.
How to prevent Achilles tendinitis
Although you cannot completely prevent Achilles tendinitis, you can reduce your risk.
- Increase activity levels – in terms of both duration and intensity – gradually. This gives your body time to adjust to the demands you place on it.
- Try to limit the amount of stress you place on your Achilles tendon by limiting running on hills and warming up well before you begin exercising. When you feel pain, stop and rest. If the pain persists, it may be time to talk to your doctor.
- Wear supportive footwear designed for the activity you’re performing. Our blog post, Choosing the Right Shoe for Your Activity, describes the ideal foot gear for a variety of sports and exercises.
- Stretch your Achilles tendon and calf muscles regularly, not just before and after exercise.
- Develop stronger calf muscles to better support your body’s weight.
- If you do a lot of high-impact activities, like running or jumping, make sure to spend some time on low-impact aerobics as well, such as bike riding or swimming.
Achilles tendinitis treatment
Most people who have Achilles tendinitis respond well to non-invasive treatment, such as over-the-counter medications and RICE:
- Rest
- Ice
- Compression
- Elevation
Your podiatrist may also recommend custom orthotics, which will elevate the heel to relieve stress on the tendon. They may also recommend exercises that help strengthen and stretch the Achilles tendon and surrounding tissues.
If conservative treatment fails, or if the Achilles tendon tears, you may need surgery.
Videos
After a lifetime of pain due to flat feet, one patient shares his experience of flat foot reconstruction surgery with Preferred Foot & Ankle.
When diagnostic tests reveal a tear or rupture of the plantar fascia, surgery may be needed to regain full function in the foot.
In this video, Dr. Brent Weintrub busts one of the most common myths about foot fractures: That if it doesn’t hurt, it can’t be broken.